How to Find a Pelvic Floor Physical Therapist
That Fits Your Needs
If you’ve been googling “pelvic floor PT near me” and feeling overwhelmed by the options, you’re not alone.
Whether you’re navigating postpartum healing, dealing with incontinence, or managing persistent pelvic pain, finding the right pelvic floor physical therapist can feel confusing, intimidating, and more personal than most healthcare decisions.
So let’s break it down.
Why Pelvic Floor Therapy Feels So Hard to Find
Here’s the truth:
Most people don’t even realize pelvic floor therapy is an option until they’re already struggling.
And once they do start looking, they often run into:
Generic clinics that barely mention pelvic health
Providers who treat symptoms, not root causes
Or worse, dismissive care that leaves them feeling unheard or even ashamed
If you’ve ever thought “I wish someone told me this sooner”, you’re exactly who we’re here for .
What to Look for in a Pelvic Floor PT
You deserve more than a 10 minute consult and a printout of kegels.
Here’s what actually matters when choosing a pelvic floor physical therapist:
1. Specialization in Pelvic Health
Not all PTs are trained in internal pelvic floor work. Look for a licensed provider who specializes, not just dabbles, in pelvic health, especially if you’re dealing with prolapse, pain, or postpartum recovery.
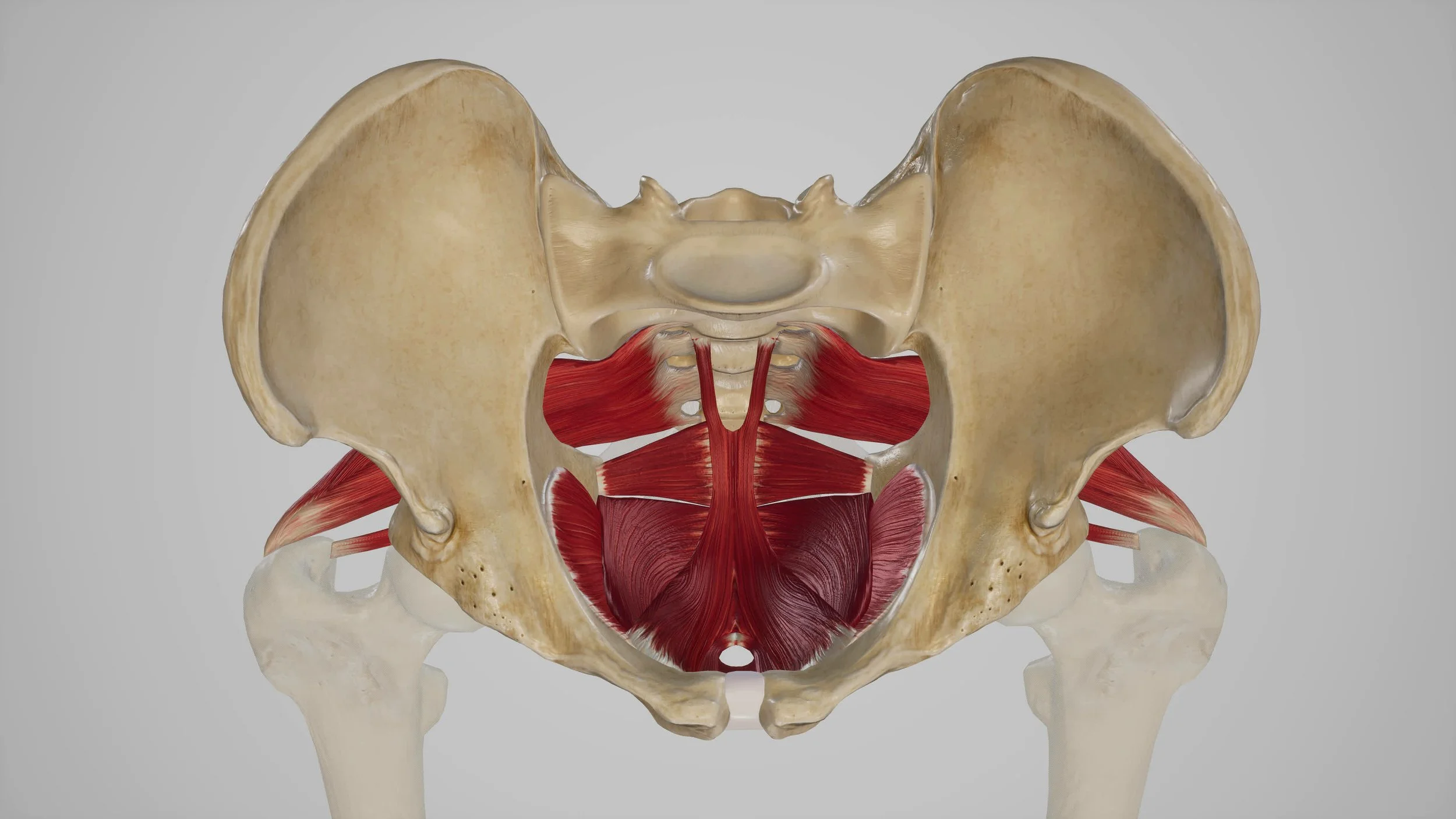
2. Whole Body Approach
Your pelvic floor doesn’t operate in isolation. It’s connected to your breath, posture, spine, hips, and even your emotional well being. A skilled therapist will assess and treat your body as a system, not just a symptom.
3. Comfort and Consent
Pelvic floor therapy can be intimate. You should never feel rushed, pressured, or uncertain about what’s happening. Look for someone who explains clearly, asks for consent, and makes space for your questions and boundaries.
4. Education Focused Care
You deserve to understand what’s going on in your body, and how to heal it. The right PT will empower you with tools, language, and clear guidance for recovery .
Questions to Ask Before Booking
Not sure how to vet your options? Here are a few questions we wish more people knew to ask:
Do you specialize in pelvic floor therapy, or is it just one of many services?
Will my sessions be 1:1 and fully private?
How do you handle internal exams and are they always required?
What’s your approach to postpartum healing?
How do you include education in your care?
If a provider can’t answer these confidently (and kindly), keep looking.
What Makes Care at Klein PT Different
At Klein Physical Therapy, we’ve created the kind of care we wish more people had access to:
Full body assessments that treat the root, not just the symptom
One on one sessions in a calm, private setting
Evidence based treatment with deep empathy and dignity
Faith informed care for clients who value that lens
We specialize in pelvic health, women’s wellness, and spine care, helping you reclaim confidence, comfort, and clarity in your body.
You’re Not Alone, And You Deserve Better
Pelvic pain, incontinence, or postpartum struggles may feel isolating, but they’re incredibly common.
And with the right care, they’re also incredibly treatable.
You don’t have to settle for being dismissed, confused, or told “this is just part of motherhood.” or “this is just part of being a woman”
Ready to Heal with Clarity and Care?
If you’re in the Denver area and looking for pelvic floor therapy that truly meets you where you are, we’d love to support you.
Book your first session at Klein PT
Or reach out with questions, we’re here to help you feel seen, supported, and strong again.